The “Moneyball for Medicine” statistic was invented a long time ago. It was invented by an Anesthesiologist with an undergraduate degree in mathematics and by an Emergency Medicine Physician with an undergraduate degree in economics. It combines the math of medical statistics with the math of economics.
The “Moneyball for Medicine” statistic is the “expected net treatment benefit for the patient using the outcome measure most important to the patient.” It’s the long-needed statistic that puts the patient first.
What do you need to know when you get sick?
- You need to know your diagnosis
- You need a list of all possible treatments
- Then you need to know the “expected net treatment benefit” from each treatment for someone like you.
We call the “expected net treatment benefit for the patient, based upon the outcome most important to the patient,” the Treatment Score. The higher the Treatment Score the better for the patient.
The Treatment Score is calculated using all three steps of evidence-based medicine:
- The medical literature
- The physician’s knowledge
- The values and preferences of the patient.
Note that the patient can’t be left out of evidence-based medicine. The patient is the essential third step of evidence-based medicine (EBM). Evidence-based medicine is supposed to be personalized and individualized. The Treatment Score makes Evidence-based medicine quantifiable down to one number, making treatments understandable at a glance, and creates the ability to do real value-based care. The overall concept is simple and would look like this on your smart phone:
This table is saying that Treatment 1 is 100% effective and Treatment 5 is 0% effective for whatever outcome measure you are using. This organizational system can be used for curing cancer or resolving the symptoms of the common cold.
Here’s What the Future Should Look Like
You suffer from insomnia. You go to the physician and he or she says pulls out their smart phone and says, “Here’s a list of all 498 treatments for insomnia (from WebMD) and to the right of each treatment is the Treatment Score as calculated by me, using my values and preferences.”
You can see the same list of treatments and Treatment Scores on your smart phone, and you can learn to adjust them based upon your values and preferences with the help of your physician to complete the third step of evidence-based medicine.
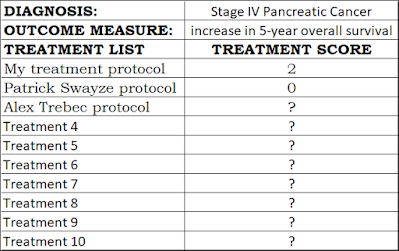
Pancreatic Cancer
Perhaps you are diagnosed with stage 4 pancreatic cancer, which is a lethal, horrible, cancer. Actor and celebrity, Patrick Swayze, died from it. The five-year survival is 1% (Johns Hopkins) and most patients don’t even live as long as one year.
Alex Trebek of JEOPARDY made it through his one-year milestone (he posted this). Mr. Trebek should have been able to scroll through a list of treatments with Treatment Scores as calculated by his treating physician on his physician's smart phone. Then, Mr. Trebek should have been able to consider his values and preferences as a patient on his smart phone, with and without, his physician, and adjust his Treatment Scores. His physicians probably did something like this, but they probably did not quantify their thinking down to one number as we need to do now for all medical treatments, and they probably did not quantify all the side effects with a trail of data to show how they got their numbers and why. Mr. Trebek died on November 8, 2020, so he survived less than two years after diagnosis.
Quantification disrupts every industry it touches. Quantification will change healthcare forever. Let’s expand our example to see what pancreatic cancer might look on your smart phone where it could fit inside two columns:
What is this table saying? It is saying that the Patrick Swayze protocol had a 5-year overall survival increase of 0% based on his one example. Patrick Swayze died 20 months after his diagnosis of Stage IV pancreatic cancer, according to various reports, so he did not make it to five years.
This table is saying we won’t know the 5-year Treatment Score for Alex Trebek because his five-year anniversary of being diagnosed won’t be until March 4th, 2024. We hope he breaks through that milestone!
My treatment protocol has an “expected net treatment benefit” = Treatment Score of 2% for increasing my 5-year overall survival if I’m lucky. I got my treatment protocol from reading the medical literature, getting my physician’s advice (me), talking to other physicians, and by using my values and preferences. Thus, I used all three steps of evidence-based medicine to calculate my Treatment Score. I don’t have pancreatic cancer; I just worry about getting it! Like many statistics, my Treatment Score has a range, and because stage IV pancreatic cancer is so deadly part of that range is below zero, so I, like most people, might not live five years. It may turn out the Treatment Score would be zero for me like it turns out to be for most people. However, at least I would have made my decision using the best data available, and would have used evidence-based medicine that was personalized to me. (Note, I am not actually claiming that “my protocol” is a hard science EBM score that is positive at 5-years; this is just an example.)
My treatment protocol would be much different from what Patrick Swayze did or from what Alex Trebek did, because as a physician, I am much more focused on quality of life rather than length of life, because I have seen the horrible side effects cancer patients suffer from their treatments. This is not an uncommon attitude among physicians. I have known cancer patients who were so miserable from their treatment that they did not want to live after being treated, even though they survived. I do not want to go through that kind of suffering. There are definitely cases where the Treatment Score is statistically likely to be negative, meaning harmful, for a cancer treatment, and I will avoid all those treatments like the plague.
It’s very telling that the Pancreatic Cancer Action Network (PanCAN), “strongly recommends clinical trials….” Even they are basically saying nothing works, at least not at the 5-year mark. Once we figured this out, we would shift our main outcome measure to 1-year overall survival. This has to be done for many of the deadliest cancers to get a positive Treatment Score.
Surely, you can see that not having a list of treatments with Treatment Scores done right now and available to all patients on the Internet is a catastrophe. If you get diagnosed with stage IV pancreatic cancer, as a patient it could easily take you a year to do your research, read all the studies, get all the advice you can, and figure out how you want to treat it. But by 1 year, about 80% of patients will be dead.
Steve Jobs
Steve Jobs was diagnosed with stage 1 neuroendocrine pancreatic cancer, the most curable type. Mr. Jobs, according to reports and books about him, underwent many treatments. Please take all these with a grain of salt even though I have references at the end, because Mr. Jobs is not here to explain what he did and why, or if he actually considered these things to be treatments. Reportedly, Steve Jobs may have done things like:
- vegan diet
- acupuncture
- herbal remedies
- psychic therapy
- organic herbs
- juice fasting
- bowel cleanings
- hydrotherapy
- expression of negative feelings
Using the hard science rules of evidence-based medicine, which require high quality studies in human beings, many of things Steve Jobs may have done according to various reports (which may or may not be accurate), would have had a Treatment Score of zero.
The possible irony and tragedy of Steve Jobs’ death cannot be overlooked. If our current system can’t explain medical statistics to an intelligent, high-tech person, such as Steve Jobs, then we have failed. Monday morning quarterbacking is easy, but we need to ask ourselves, “Would Steve Jobs be alive today if he had had Treatment Scores?” If Mr. Jobs had understood the medical statistics? The irony is that one of the inventors of the hardware, the iPhone, that is changing healthcare did not have the software on it, Treatment Scores, that might have saved his life. But we are guessing, because no one I personally know has the details of his situation, nor does anyone know if the disease would have progressed regardless of treatment.
We can honor Steve Jobs posthumously by listening to what he said: “You've got to start with the customer experience and work back toward the technology—not the other way around.” Steve Jobs, (May 1997, World Wide Developers Conference). This is what we need to do with Treatment Scores.
Mathematics
You can click on each Treatment Score and follow the trail back to where it originated, and you can study every value, calculation, and reference along its path. The Treatment Score combines the math of medical statistics with the math of economics, and digests it all down to one number. Here’s one conceptual example of the math involved:
- 1 diagnosis
- 10 possible treatments for that diagnosis
- 10 vital statistics for each of those treatments
- 10 references used to get those 10 vital statistics
- 10 pieces of data for each reference.
That's 10×10×10×10 = 10,000 pieces of information that must be processed and transformed into a Treatment Score. Yet, with computers it can all be quite simple. We have already created working software to do it.
Let’s explain it simply. If you run a business, every year you need to know your “net income” for that business. Of course, you start with your “gross income” to get to your “net income.”
The same thing for taxpayers doing their taxes every year. You have to start with your “gross income” and figure out your “net income” to pay your taxes.
The formula is: gross income – expenses = net income.
For medical treatments the formula is: gross treatment benefit – negative side effects = net treatment benefit.
It’s more complicated with medical treatments because there can be “side benefits” to a medical treatment. For example, proponents of medical marijuana for treating nausea from chemotherapy will often mention the side benefit of medical marijuana treating pain as well. There are many examples of medical treatments that have both negative side effects and positive side benefits. The formula becomes:
Gross treatment benefit – side effects + side benefits = net treatment benefit.
Subtracting the side effects is extremely important. There are patients who say that being incontinent of feces, or incontinent of urine, would be worse than death for them. There is a brain tumor surgery that can cause a complete and horrific paralysis of one side of the face. Many patients say that this side effect would be worse than death for them. Many patients would subtract a lot for the side effect of peripheral neuropathy—which can be a constant painful side effect of the skin for the rest of one’s life.
“Side benefits” cannot be overlooked either. Many people think chronic pain patients are being crucified by “medical guidelines,” which are not evidence-based medicine, but are only step 1 of EBM. A pain pill may decrease pain, but it may also have very important positive side benefits:
- Enabling the bedridden to get out of bed
- Increasing all physical activity
- Decreasing suicidal ideation
- Decreasing suicides
- Increasing mental clarity
When treating a chronic pain patient, like somebody who has had four failed back surgeries, you must add these positive side benefits into the equation to get an accurate Treatment Score. You can’t just focus on the well-known negatives. Doing Treatment Scores would greatly help to sort out the management of chronic pain patients. Treatment Scores would ensure that the values and preferences of the individual patient are included.
Insomnia
Let's speak again of insomnia again. So many people have trouble sleeping! There are 498 treatments for insomnia listed on the WebMD website. So the math is like this:
Diagnosis: Insomnia
- 498 treatments
- 10 vital statistics for each treatment
- 10 references for each vital statistic
- 10 pieces of data for each reference
That's 498 x 10 x 10 x 10 = 498,000 pieces of data that must be summarized into Treatment Scores using evidence-based medicine guidelines.
This is why we need computers. One diagnosis can have about half a million (500,000) data points that must be incorporated. Fortunately, we have everything we need to create understandable treatment transparency for patients: the Internet, new database technology, and new medical statistics.
The Money Example
This simple equation:
Gross treatment benefit – side effects + side benefits = net treatment benefit, still confuses people. It’s because all of these things are on different scales and have to be converted to be on the same scale.
It’s like our main outcome measure is in dollars, but our side effects are in other currencies such as pesos, British pounds, and Euros. With Treatment Scores, math is used to create conversions for all side effects and side benefits so that they can all be put on the same scale. These conversion factors come from patients, so again, Treatment Scores put the patient first!
Here is a graphic of calling the main outcome measure, perhaps 5-year overall survival, “dollars,” to help with the flow of doing conversions to get the main outcome measure, the side effects, and the side benefits all on the same scale:
Remember, we are just taking the outcome measure most important to the patient, such as 5-year overall survival, and are converting the side effects and side benefits onto that same scale so we can summarize the treatment into one number. It’s like adding up dollars, pesos, British pounds, and Euros, where “dollars” actually stands for 5-year overall survival, or some other outcome measure important to the patient.
57 Treatments that Don’t Work
Patients often undergo medical treatments without realizing they have almost zero chance of helping them.
During their 4.4-year study, Chul Kim, MD, MPH, and Vinay Prasad, MD, MPH, found that 31 FDA approved chemotherapy drugs did not improve overall survival or had no solid proof they improved overall survival.
In other words, 31 medications had a Treatment Score of zero! Maybe less than zero because of their side effects. Yet, all these treatments can be used, and can be reimbursed, because they are FDA approved. I do not think that a treatment that works 0% of the time, according to evidence-based medicine, for the outcome I want should be reimbursed at the same rate as a medication that works 99% of the time. Sadly, this is how the system currently works.
Cancer Scams
Here’s how a “cancer scam” works even in the best, most legitimate, places. Someone tells the patient they have cancer. Then they proceed to “scare the hell out of the patient,” as the idiom goes. The patient becomes very afraid. The medical industrial complex with its information monopoly throws in frightening words about what could happen: death, metastases, pain, agony, and so forth.
But it may be one of those cancers that is unlikely to ever kill you. You may have no idea, you just know “cancer!” You keep hearing the word: cancer, cancer, cancer, bounce around inside your head. The patient is led into making an emotional decision based on fear and does harm to themselves financially (a wallet biopsy), and physically because of horrible side effects, when there were better options. If the patient had understood the situation, they might have made different choices. Some people get very rich off of this information monopoly. Search “overtreatment” and you will find over 1.5 million results, and not just for cancer.
Paternalistic Medicine is Bad Medicine
In healthcare, the default has been to just have the doctor tell you what to do—paternalistic medicine. Yet, paternalistic medicine has been declared unethical many times. After the epidemic of unnecessary hysterectomies performed on women, paternalistic medicine was declared unethical. Paternalistic group-think medicine was declared unethical after many patients were given antiarrhythmic drugs only to have independent studies prove later that the drugs were killing people. Paternalistic medicine was denounced at the Nuremberg Trials in favor of informed consent, which means shared decision-making with the patient. Tragedies like these are why we want every doctor and patient to be able to go to the data themselves and evaluate it, using software. You must be your own best healthcare advocate and your doctor must put you first.
We are still doing far too much paternalist medicine. In the old days, the doctor told the patient what to do. These days, someone writes guidelines telling doctors what to do, and then the doctors tell the patient what to do according to the guidelines. It’s paternalist medicine one step removed. Guidelines are dressed up as evidence-based medicine, but they are only the first step of evidence-based medicine, a review of the medical literature. Guidelines, systematic reviews, and meta-analyses are not evidence-based medicine, as without the last two steps: the physician’s input and the patient’s values and preferences, EBM is not complete. Search “critique of meta-analyses” and “critique of guidelines” and “critique of systematic reviews” and you will find well over 1 million search results.
It is hard to emphasize this enough, “medical guidelines” by Academia, Government, or Industry, are not evidence-based medicine, because they do not necessarily include the essential second and third steps of EBM, the physician who knows the patient the best, and the individual patient. Guidelines leave out the individual patient’s values and preferences and guidelines are not personalized medicine or individualized medicine.
Bias in the Medical Literature
The bible roughly says, “the love of money is the root of all evil.” Notice the importance of the word “love.” Some people can act in a logical and unbiased manner regardless of money and some cannot. Money in and of itself is a tool, not an evil.
Power is similar, it can be good or bad. “Power corrupts: absolute power corrupts absolutely,” was an observation by Lord Acton (shorted by me). Lord Acton was a politician born in 1834 and he warned us!
In short, money or power can cause bias in the medical literature, and there are three main sources of bias in the medical literature:
- Academia
- Government
- Industry.
Treatment Scores account for all of these biases. One way to counter these biases is transparency. Ideally, at the end of every medical study there should be a box for all three of these biases, and every author should check the appropriate box, or boxes, and declare all money received in their lifetimes up to the point of writing their study from these sources. Many doctors are totally unaware of the “dark” or “hidden” money they have received during their lifetimes and its subtle influence. Medical students and residents are particularly clueless in my experience.
These statements are somewhat true: “You can buy a scientist just as easily as you can buy a politician,” and, “You can buy a physician just as easily as you can buy a politician.” There is actually more transparency about politicians than about scientists or physicians, so the bad politicians are more visible. I have met many scientists, physicians, and politicians, and the majority are great, smart people, but just like in all other walks of life there are some bad actors. This is why Treatment Scores emphasize mathematics and minimizes human bias.
John P.A. Ioannides, MD, DSc.
Those of us who love math and hard science admire John P.A. Ioannides, MD, DSc., who famously wrote the article, “Why Most Published Research Findings are False.” We like Ioannides because we believe he is right. Medicine consists of a mountain of bad studies and a tiny hill of good studies.
Who should Calculate Treatment Scores?
Why the emphasis on bias? Because there is tremendous bias in the medical literature. The ideal study is an unbiased, double-blinded, randomized controlled clinical trial, because the very purpose of a randomized controlled trial is to remove bias. Guidelines, systematic reviews, and meta-analysis done by humans can put bias back in.
The ideal review of the medical literature would be done by an unbiased physician. Systematic reviews and meta-analyses are not unbiased, and I am not aware of an unbiased, double-blinded, randomized controlled clinical trial that proves that either a systematic review or a meta-analysis is better than an unbiased, double-blinded, randomized controlled clinical trial. Please re-read that! Have we adopted something as a new “Gold Standard” without doing the science to prove that it is a new and better Gold Standard?
The next step in the evolution of medical information should be the “expected net treatment benefit” for the patient, using the outcome most important to the patient, done in an unbiased fashion, using math as much as possible, because math doesn’t lie and math can remove bias.
You want physicians who are independent of Academia, Government, and Industry calculating Treatment Scores. You want independent physicians who are working directly for patients without any third parties (Academia, Government, or Industry) standing between the doctor and patient. If such third parties are involved, they need to disclose their past money from all three sources. This moral code should be obvious, but it is not. As a patient, you do not want third parties influencing physicians’ decisions.
Journal Clubs
I have talked to many residency directors and resident physicians about Treatment Scores, and I can’t believe what I have heard! One Ivy League residency program is thinking of abandoning Journal Club altogether. Journal Club was one of my favorite parts of residency. Journal Club is important because you review all the latest medical studies and figure out what information is good enough to use. You also learn how to “Study a Study.” Residency directors have told me that nobody shows up for Journal Club, or they have to bribe residents with free food. This is wrong. All residency programs should be calculating Treatment Scores during Journal Club. Journal Club is life and death important.
Medical School Applicants
We should be choosing students to enter medical school who are great at mathematics, medical statistics, and who are good at computer programming. We need to move in the direction of unbiased medical informatics to have a better future. Sadly, many studies show that patients are health illiterate, and worse, physicians are illiterate when it comes to medical statistics. The blind really are leading the blind!
Tumor Boards
Many hospitals have a “Tumor Board,” which is a group of physicians that get together and go over the laboratory results and scans for the patient that has cancer and decides, as a group, how to treat the patient. These Tumor Boards are often an expert team with a pathologist, an oncologist, surgeon, and a radiation oncologist. All Tumor Boards should be creating Treatment Scores and publishing them for public peer review. This would take medicine out of the dark ages and into the light as the patient would finally be able to see what is happening in the real world.
Medical Research
Medical research should be based on Treatment Scores. Right now, the way money is given to the National Institutes of Health is very political. There are hearings and those who scream the loudest and obtain the most political power are often the ones who get the money. If we had Treatment Scores for everything, we could go down the line and fund the deadliest or most disabling diseases that have treatments with the lowest Treatment Scores. There could be more logic to the process. We could also identify where private industry needs to innovate.
Roll Back Regulations
We need to make physicians scientists again. We need to roll back the regulations that prevent physicians from having a microscope! All primary care physicians need a laboratory and the tools to do ethical clinical research. Especially research on things like Treatment Scores. All primary care physicians should be calculating Treatment Scores before treatment, and should also be getting follow-up Treatment Scores after treatment.
“Doctor, what would you do?”
What the patient typically wants to know, and needs to know, is the answer to the age-old question, “Doctor, what would you do if it were you?” I heard this question asked by patients many times during medical school and residency to my attending physicians. It has been asked of me many times.
This question by patients really gets to the heart of the matter. If your doctor drops all biases, conventional wisdom, and ignores what is commonly done because it’s always been done, and focuses on what they would do for themselves after calculating Treatment Scores, what would it be? It would often be something different than what you get.
Getting the answer to “Doctor what would you do?” gets you to step 2 of evidence-based medicine. Then, the doctor and patient need to sit down and do step 3 of evidence-based medicine, the patient’s values and preferences, to get the final Treatment Score.
Who’s Looking over Your Doctor’s Shoulder?
Anesthesiologists have surgeons looking at their work every day all day long. Emergency Medicine physicians have their work reviewed every time they refer a patient on to another physician. The same for Family Medicine physicians.
But who is looking over the shoulder of your urologist? Your neurosurgeon? Your endocrinologist? Often, no one independent of their specialty is checking if what they do is scientific and logical.
Treatment Scores fixes that. Treatment Scores create “public peer review” and allow other doctors, and all patients, to review the science and logic behind medical treatments. This kind of medical transparency is priceless and badly needed—yesterday.
Family Medicine physicians, Emergency Medicine physicians, Pediatricians, and all primary care specialties should be reviewing and critiquing the Treatment Scores done by the urologists, neurosurgeons, oncologists, and endocrinologists. They should be checking the Treatment Scores of the physicians they refer patients to. And, instead of referring patients based on hospital rotations (politics) as is done now, they should refer patients based on the best treatment available according to Treatment Scores, regardless of the specialty. For example, every prostate problem is sent to a urologist, because they “own” that organ. Yet, the best treatment and the highest Treatment Score for a specific patient might be with an oncologist who does active surveillance.
We need to complete the circle of quality control. It should not be a straight line from primary care to specialists. It should be a circle from primary care to specialists and back to primary care. There needs to be a Family Medicine revolution.
Quality Control Example
There is a great example in medicine where a surgeon claims the surgery that he does for cancer has a 90% cure rate. Looking at the exact same data, physicians, who don’t do the surgery, in other specialties think the operation has a 10% or less Treatment Score. Furthermore, this debate has been going on for 22 years without the data changing significantly, because the newer studies also show the 10% or less Treatment Score. But most of the world cannot understand this situation, because the data is not transparent. If this data were organized and summarized into a Treatment Score, far more people would understand that the surgeon is including patients that don’t need to be cured in his data, while the other physicians only include patients that need to be cured from this slow-growing cancer.
This is why having different specialties doing Treatment Scores will be so important. It removes bias. If the specialty of surgery does a Treatment Score and it is very high, and the specialty of anesthesiology does a Treatment Score for the same treatment and it is very low, there is a problem! This kind of quality control reveals bias, bad data, missing data, or some other problem. Patients need to know this information!
Public Peer Review
Treatment Scores create the ability to do “public peer review” and to teach patients how physicians think when they use science and logic. Logic starts at the beginning. What is the highest quality, most relevant study, for the diagnosis and treatment being studied? That’s where Treatment Scores start.
Follow-Up After Treatment
Patients, using shared decision-making with their physician, are given the expected Treatment Scores before treatment. After treatment, we should follow-up with the actual Treatment Score with the patient reporting their actual outcome, actual side effects suffered, and actual side benefits. This is the perfect universal way to collect pre- and post-treatment data. Giving the patient the “expected” Treatment Score beforehand, and the patient giving the “actual” Treatment Score obtained after treatment. Over time the gap between “expected outcomes” and “actual outcomes” should start to narrow.
Treatment Scores should become the universal system for treatment transparency before treatment and for follow-up after treatment.
Follow the Headlines
Once Treatment Scores gets going, they will get free publicity. For example, COVID19 is dominating the news. We can calculate Treatment Scores for that!
What if the diagnosis is “preventing COVID19 in the average person?” And, the treatment list is:
- Wearing a surgeon’s mask
- Wearing a cloth mask
- Or taking the triple therapy of hydroxychloroquine, zinc, and or azithromycin as prophylaxis.
There’s a Treatment Score for all these treatments that can be put up for public peer review. And, it depends on the patient what the most important outcome measure is for them. One might start with 5-year overall survival as an outcome measure. If studies cannot be found using that outcome measure, another outcome measure would have to be chosen.
If a 6-year-old kid is sent to school wearing a surgeon’s mask all day long for one year because of COVID19, how much would it increase or decrease their 1-year overall survival? This would be an important Treatment Score to calculate. But when we dig into it, we may not have the needed studies, so we may have to use a more available main outcome measure. We will have to find the most relevant studies and the highest quality studies. Once Treatment Scores get started, they can make headlines every week by jumping on the major healthcare news story of the week and publishing Treatment Scores.
Questions we need to Answer
Treatment Scores could give quantified answers to all of these questions, and put them up for public peer review. Treatment Scores would also allow each question to be answered with personalized and individualized medicine, which has long been the goal.
- Should you wear a cloth mask to prevent getting or spreading COVID-19?
- Should you make your child wear a mask all day long every day at school?
- If you get COVID-19, should you take remdesivir?
- If you get COVID-19, should you take hydroxychloroquine + azithromycin + zinc?
- If you get COVID-19, should you take steroids via an inhaler?
- If you get COVID-19, should you take steroids as intravenous dexamethasone?
As you can see from looking at the world today, we can’t even organize the medical literature into the highest quality and most relevant studies for any clinical question for the public, patients, doctors, and nurses. Treatment Scores would fix all that.
What is the single best study to answer each of these COVID-19 questions? Logic says we need to start at the beginning, at the single best and most relevant study. Where is that study? What does it say? Why don’t you know after all these months of a lethal pandemic?
Obstacles to Moneyball for Medicine
1. Apathy. Most people are not sick most of the time, and most people don’t want to think about getting sick. This creates a great deal of apathy. However, the healthcare industry is a 7-trillion-dollar industry worldwide, so it is tremendously significant. Demand will change. Once patients can look up a list of treatments with Treatment Scores for the common cold, they will want to be able to do it all the time for all diseases, and they will be surprised by what they find.
2. Quantification is a sea change. We have to turn the Titanic to create treatment transparency and it will require momentum. At first the status quo in Academia, Government, and Industry will resist this change, they already have.
3. Time. Treatment Scores will take an enormous amount of time by highly intelligent physicians and programmers at first, but will get faster and easier with time as the system is built.
4. Health illiteracy. Most patients are health illiterate. And, as my physician colleague, a Family Medicine physician said to me, “They are also just plain math illiterate.” We need patients to demand Treatment Scores. There are 57 treatments in the medical literature for an acute migraine headache. Why don’t we have a list of all 57 treatments with a Treatment Score for each one? One reason is that patients don’t demand better treatment transparency. Patients don’t know that they need to demand this type of organization and quantification with Treatment Scores, but eventually they will. You are the agent of change.
5. Most doctors are not hard scientists, and most doctors, according to studies, are not very good at medical statistics.
6. The status quo. It is hard to improve healthcare, because the current third parties are making money hand over foot and are enjoying incredible power far beyond what they deserve. Data science has not done its job. Medical informatics has not done its job. Continuing Medical Education (CME) should be all about Treatment Scores. Bill James invented Sabermetrics for baseball, which led to the book and movie, Moneyball, and the entire process of invention to adoption, leading to a World Series victory, took 20 or 30 years.
Ethics. Why haven’t Treatment Scores for every medical treatment been done yet? Some have been done, but another hurdle is ethics. To produce Treatment Scores, we need doctors that want to put the patient first. We need doctors that want to end the information monopoly that exists now, where physicians know everything (or a lot) and patients know next to nothing. Patients need transparency: both price transparency and product transparency. When you translate product transparency from economic terminology into medical terminology, you get “treatment transparency.”
Ethics in business. We also need business people that want to do the right thing. There is so much secrecy in medicine now, things hidden from patients, that the system makes out like a bandit from secret monopolies. The people making excess money from secrecy don’t want to see the system changed.
Brain power. The first time Treatment Scores are done for any diagnosis, it takes a lot of brainpower and time by human beings, because you have to start with a systematic review and meta-analysis of the literature, which according to one study takes on average, 5 people working for 67.3 weeks (Borah). However, once the Treatment Score is done the first time, computers come into play, and algorithms can be used to constantly keep the Treatment Score up to date, and crowd wisdom can be used to keep checking for problems in the data. Time is also saved because once done, a good Treatment Score does not change much over time. I calculated a Treatment Score of less than 10% in 1998 for a certain surgery, and that Treatment Score has not changed in 22 years. This is because once a really good randomized controlled trial proves something, future good studies reinforce that finding—they don’t change it.
Salaries. To get Treatment Scores going, one would need to hire a super smart, logical, and creative physician away from their already highly paying job, and would need to hire an excellent, already highly paid programmer, who hopefully is a physician as well (yes, a few of them exist), and then be able to pay them for years to develop Treatment Scores.
Revenue Streams. An incredibly user-friendly smart phone app would need to be created that would be so simple that all physicians and all patients could use it. Revenue streams would have to be created. Since Treatment Scores would steer everyone in the healthcare system to treatments that tend to work, and away from treatments that are highly questionable, this would lower costs in the entire healthcare system. Treatment Scores would also make it apparent when two medical treatments have the same outcome for patients, yet one costs 1 million dollars while the other treatment only costs $10,000.
After Treatment Scores get going, the backend can be infused with artificial intelligence, which will automate things more and more until the entire process of 10,000 variables becomes incredibly fast.
We all need to insist that medical studies be more machine-reader friendly! Natural search engine technology is doing this for us, but the publishers need to start doing it. We need to be able to find the best studies more easily, so they need to be better labeled. In addition, I often find a data point that I need in a study, but I have to calculate it by hand, because the authors don’t place enough importance on this finding in their own data.
Treatment Scores will Happen
Quantification of medical treatments will happen. Treatment Scores have to happen, because they will improve healthcare by leaps and bounds. I think we will look back one day and see the quantification of healthcare with Treatment Scores as being more important than the invention of Penicillin. The good of penicillin has mostly come and gone as bacteria have developed resistance to it, and because many other antibiotics have been invented that can be used instead. However, the good of Treatment Scores to organize and quantify medical treatments (and all clinical decisions) will go on forever.
Someday, a simple Treatment Scores smart phone app is going to change everything about healthcare by shining a light into the darkness.
What Should Drive Treatment Scores
1. Better patient outcomes. Treatment Scores will solve the problems of health illiteracy, undertreatment, and overtreatment. Because Treatment Scores measure value as determined by the patient, not some uncaring third party, patient care can be improved for the patient. Treatment Scores will mean better patient care at a better price, because less money will be wasted.
2. Passion & Panic. When people do get sick, they are often consumed with passion to get well. They spend boundless time and energy trying to get better. This is the time, if patients realize how Treatment Scores work, that they will desperately want them. Patients may have to drive Treatment Scores. A patient may get sick with colon cancer, breast cancer, or prostate cancer and may passionately want to know the list of treatments and Treatment Scores. Perhaps a start-up company will provide them for the patient on their smart phone. That patient then needs to be able to share that same list of treatments with Treatment Scores with their physician so they can do steps 2 (physician expertise) and step 3 (the patient’s values and preferences) of evidence-based medicine.
3. Desire to help people. Most doctors truly want to help people. They can maximize the good they can do with Treatment Scores. When doctors understand what Treatment Scores can do for them, they will want them.
4. Healthcare is going broke. Treatment Scores can lower costs and improve care simultaneously, and for all parties in healthcare, patients, doctors, nurses, allied healthcare professionals, hospitals, insurance companies, and governments.
5. Non-profits. My friend got a particular kind of breast cancer. It was not my area of expertise, so I called a breast cancer non-profit. I said, “The patient has stage 4 breast cancer with these other markers and characteristics. What are the treatments that should be on the list of treatments for this?” Dead silence. I was incredibly polite, but ended up being met with hostility. We need to change it so non-profits can be curators of a list of treatments with Treatment Scores. Most of them have physicians and highly, highly intelligent patients they work with. Non-profits should be able to curate a list of treatments with Treatment Scores and give the simple disclaimer, “We do not recommend any specific treatment, but when we do the math for ourselves, we get this.” This inside knowledge should not be hidden from patients.
How to get Started
A super simple and easy smart phone app needs to be created. That’s going to take a programmer, hopefully a physician programmer, who can work with at least one physician who knows how to create Treatment Scores. So, right off the bat, there needs to be salaries for at least two brilliant people, who already have salaries that would be difficult to give up. Because of COVID-19 these people probably need to work at home, so the entire system of doing Treatment Scores, conferences, and teaching should probably be set up as telemedicine/videoconferencing from the beginning.
Licensing
The people most interested in Treatment Scores right now are the patients smart enough to understand the entire concept. But once a large group of patients understands Treatment Scores, there will be a large demand for them. There should be a revenue stream created by producing a yearly book of Treatment Scores for all diseases and all treatments, and those scores can be tied to reimbursement, and done so fairly, because the scores are produced with input by the patients themselves. The licensing fees for using such a database for reimbursement should be astronomical, because Treatment Scores are much more important than many other medical codes that are licensed. After all, treating patients to make them better is the main point of healthcare.
Change will occur. Understandable treatment transparency, quantified, for the patient is too good of an idea to ignore forever. One day, Treatment Scores will change the world. The good of knowing the “expected net treatment benefit for the patient” cannot be denied.
Spokesperson
The ability of Treatment Scores to ride the wave of every health-related news cycle means that Treatment Scores must have a great spokesperson for the media. As I am fond of saying, “People don’t believe statistics; people believe people who can explain statistics.”
Who Needs Treatment Scores?
Who needs Treatment Scores? Patients, doctors, nurses, all allied healthcare professionals, all medical schools, all medical residency programs, all hospitals, and all medical research entities. Pretty much everyone needs Treatment Scores at some point including all insurance companies and governments.
Perhaps there will be a start-up that uses independent physicians to calculate Treatment Scores. Patients will want these Treatment Scores once they understand them, because their life is at risk, and their health is at risk, and they need a trusted source of information. COVID19 has taught us that this work can be done remotely. Telemedicine/video-medicine is great for Treatment Scores.
Perhaps a business will start-up to do Journal Clubs remotely for all medical residency programs. All resident physicians should be doing Treatment Scores. Why not create the app so that they can actually do them? Why not collect all that data and start improving treatment transparency and start doing better quality improvement in healthcare? We need to solve health illiteracy and we need better patient care.
Every physician should carry on their cell phone a list of treatments with Treatment Scores for all the diagnoses that they deal with most often. Algorithms should help the physician keep the Treatment Scores up to date. An alert should be sent out when a good study changes a Treatment Score. It should not take years and years to filter through the medical system. The sick patient should have the same list of treatments with Treatment Scores on their cell phone so that they can be their own best healthcare advocate. We could have individualized medicine, because every individual’s tolerance for risk is different and medicine needs to be personalized. Treatment Scores will:
- Put the patient first
- Improve patient care
- Decrease costs
- Enable true value-based healthcare using patient preferences
- Improve treatment transparency • Help solve health illiteracy
- Save time for patients, doctors, and nurses
- Make your smart phone even more important for healthcare.
References:
Bruce Ramshaw, MD. “Moneyball for Health Care: Why Hasn’t it Happened?” General Surgery News (July 29, 2020). This article also appeared in Healthcare: Systems Science (August 17th, 2020).
Rohit Borah, Andrew W Brown, Patrice L Capers, Kathryn A Kaiser. “Analysis of the time and workers needed to conduct systematic reviews of medical interventions using data from the PROSPERO registry.” BMJ Open. October 25, 2016. https://bmjopen.bmj.com/content/7/2/e012545. Accessed September 10, 2020.
PanCAN. Quote: “The Pancreatic Cancer Action Network strongly recommends clinical trials at diagnosis and during every treatment decision.”
https://www.pancan.org/facing-pancreatic-cancer/treatment/treatment-types/clinical-trials/ Accessed: September 9th, 2020.
Johns Hopkins Medicine. “Pancreatic Cancer Prognosis: Stage IV Prognosis.”
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-prognosis
Accessed September 9, 2020.
Chul Kim, MD, MPH and Vinay Prasad, MD, MPH. “Cancer Drugs Approved on the Basis of a Surrogate End Point and Subsequent Overall Survival: An Analysis of 5 Years of US Food and Drug Administration Approvals.”
JAMA Intern Med. 2015;175(12):1992-1994. Doi:10.1001/jamainternmed.2015.5868
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2463590
Accessed: September 1, 2020.
John P.A. Ioannides, M.D., DSc. "Why most published research findings are false." PLoS Med. 2005 Aug;2(8):e124. doi: 10.1371/journal.pmed.0020124. Epub 2005 Aug 30.
http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124 Accessed: September 8st, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1182327/
Jacob Sullum. “America's War on Pain Pills Is Killing Addicts and Leaving Patients in Agony.” The government's efforts to get between people and the drugs they want have not prevented drug use, but they have made it more dangerous. Reason. April 2018 issue. https://reason.com/2018/03/08/americas-war-on-pain-pills-is/ Accessed: September 16, 2020.
Steve Jobs. Quote: “You've got to start with the customer experience and work back toward the technology - not the other way around.” May 1997, World Wide Developers Conference.
WebMD. "498 medications found for insomnia."
Accessed September 19, 2020.
URLs about Steve Jobs:
https://sciencebasedmedicine.org/one-more-thing/
https://fortune.com/2008/03/05/the-trouble-with-steve-jobs/
https://healthland.time.com/2011/10/05/the-pancreatic-cancer-that-killed-steve-jobs/
https://www.nytimes.com/2011/11/01/health/hindsight-is-kind-to-steve-jobss-decision-to-delay-surgery.html
https://www.livescience.com/16551-steve-jobs-alternative-medicine-pancreatic-cancer-treatment.html
https://www.nytimes.com/2011/10/21/technology/book-offers-new-details-of-jobs-cancer-fight.html
https://www.thedailybeast.com/steve-jobs-dies-his-unorthodox-treatment-for-neuroendocrine-cancer
https://alternativemedicine.com/alternative-medicine/departments/did-alternative-medicine-kill-steve-jobs (This URL may not be active.)
CONTACT:
Dr.Hennenfent [at] gmail.com